Children at Risk of Multiple Sclerosis Often Go Undetected in Early Stages

Rutgers study finds detection tools used for at-risk adults fail to predict the neurological disorder in young patients
Criteria used by neurologists to assess for multiple sclerosis (MS) in adults may fail to identify the illness in children with imaging suspicious for the disease, an oversight that could delay treatment of the disease at its earliest stages, according to a Rutgers study.
Magnetic resonance imaging (MRI) is the primary tool used for diagnosis of MS, and doctors have applied various standards over the years to classify those most likely to develop the disease. The most recent standard, known as the McDonald criteria, was last updated in 2017.
In some cases, imaging suspicious for MS is found incidentally before the disease manifests, a condition known as radiologically isolated syndrome (RIS). But after reviewing the MRIs of children with RIS, researchers determined these criteria are likely insufficient for pediatric patients.
“In our study, not all patients met the McDonald or Barkhof criteria [the current standard for diagnosing adult RIS], yet some went on to develop MS,” said Vikram Bhise, director of Child Neurology and Developmental Disabilities at Rutgers Robert Wood Johnson Medical School, and lead author of the study published in the journal Multiple Sclerosis and Related Disorders. “This suggests that the criteria used to characterize RIS in adults might be insufficient for the younger population.”
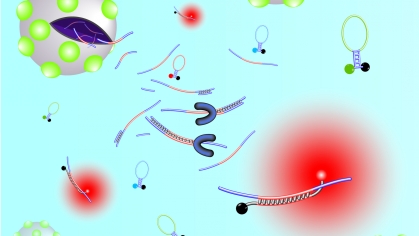
To determine if children with abnormal MRI findings would develop symptoms associated with MS, and to understand how diagnostic tools used for adults apply to children, researchers examined MR images of children suspected of having demyelination, damage to the protective myelin sheath that surrounds nerve fibers in the brain.
When the myelin sheath is damaged, nerve impulses slow or even stop, causing neurological issues. This damage appears as lesions – white or gray spots – on an MRI. There are many reasons for abnormal MRI findings; most don’t represent demyelination. While not all patients with MRI findings typical of demyelination go on to develop MS, a substantial number do.
Study participants were identified through the U.S. Network of Pediatric Multiple Sclerosis Centers and Rutgers Robert Wood Johnson Medical School databases. Patients were between 7.6 years and 17.8 years of age, and each had MRI findings that showed demyelination.
None of the children in the study had physical or neurological symptoms common to MS – such as blurred or loss of vision, vertigo or numbness or weakness in one or both legs – at the time of their initial MRI. While the database didn’t record why participants had been tested, Bhise said headaches were the most common reason.
After initial review of MRI data, patient data was assessed over a mean duration of 3.7 years to measure development of a first MS attack or new lesions. Of the 38 patients included in the study, 14 of 35 (40 percent) experienced a new clinical attack and 27 of 37 (73 percent) exhibited new MRI lesions during the review period.
When the researchers applied current MS diagnostic measures to the cohort, they found that many patients still developed MS even though they failed to meet either the McDonald or Barkhof criteria.
“Finding MS early can help a doctor knock out a whole bunch of future problems for their patients,” Bhise said. “But that can only happen with accurate diagnostic tools.”
In the U.S., an estimated 1 million people are living with MS, and about 4,000 are under the age of 18, according to MS International Federation, a global network of MS societies.