Medical School Integration: About
Find the latest updates on our progress and process, learn about the benefits of integration, and read past updates and communications.
Curriculum

Several key decisions have been made for the future Rutgers School of Medicine single curriculum by multiple working groups of the Curriculum Subcommittee.
The school will have a single set of schoolwide competencies and objectives. A clerkship curricular schedule has been developed. All preclerkship courses will be identical in content and learning modalities. Assessment and grading decisions are under deliberation.
We have identified the eight core competencies below for the curriculum.
Accordion Content
-
Demonstrates integrity, respect, and ethical reasoning, and promotes inclusion of differences in all interactions to improve healthcare for patients, communities, and populations.
Objectives:
- Student demonstrates respect and compassion for patients, caregivers, families, and team members.
- Student safeguards patient privacy, confidentiality, and autonomy.
- Student uses ethical principles and reasoning to guide behavior.
- Student adapts actions and communication according to the situation.
- Student takes ownership of mistakes and acts to address them.
- Student identifies personal limits of knowledge and seeks help appropriately.
- Student demonstrates cultural humility and a willingness to learn from others, including those with different backgrounds and experiences.
- Student recognizes and addresses personal well-being needs that may impact professional performance.
- Student completes duties and tasks in a thorough, reliable, and timely manner.
-
Demonstrates compassionate, effective, holistic, evidence-informed, and equitable patient-centered care.
Objectives:
- Student gathers relevant patient histories from multiple data sources, as necessary.
- Student performs relevant physical examinations using appropriate techniques and tools.
- Student identifies patients in need of urgent or emergent care, seeks assistance, and recommends initial evaluation and management.
- Student creates and prioritizes differential diagnoses.
- Student proposes hypothesis-driven diagnostic testing and interprets results.
- Student formulates therapeutic management plans for commonly encountered clinical conditions.
- Student uses patient-centered language to describe common diagnostic and therapeutic interventions and plans.
- Student demonstrates basic procedural techniques.
- Student incorporates health promotion and disease prevention into patient care plans.
-
Applies and integrates foundational knowledge to improve healthcare for patients and populations.
Objectives:
- Student demonstrates knowledge of basic, clinical, pathophysiologic, social, and health systems sciences, as well as humanities, needed for clinical practice.
- Student applies foundational knowledge of clinical problem-solving, diagnostic reasoning, and decision-making to clinical scenarios.
- Student discerns the accuracy of information and its relevance to clinical problems.
- Student accesses knowledge relevant to clinical problems using appropriate resources, including emerging technologies.
-
Integrates feedback, evidence, and reflection to adapt behavior, foster improvement, and cultivate life-long learning.
Objectives:
- Student actively seeks and incorporates feedback and assessment data to improve performance.
- Student identifies opportunities for growth their performance through informed self-assessment and reflective practice.
- Student locates, critically appraises, and synthesizes information to support evidence-informed, patient-centered clinical decisions.
- Student develops, implements, and reassesses learning and improvement goals.
- Student demonstrates inquiry and an ability to grow and seek new knowledge.
-
Effectively communicates and interacts with patients, caregivers, and the healthcare team to contribute to high-quality patient-centered care.
Objectives:
- Student collaborates with patients, caregivers, and team members to enhance the therapeutic relationship.
- Student collaborates with healthcare and administrative team members to enhance team and organizational functioning.
- Student demonstrates active listening.
- Student communicates clearly, accurately, and compassionately in verbal, nonverbal, written, and electronic formats, including the appropriate use of a medical interpreter.
- Student demonstrates skills to educate patients, caregivers, peers, and team members.
- Student formulates and shares feedback constructively with others.
-
Applies knowledge of the larger context of health, including its social and structural determinants, and of systems and resources within and outside of health care, to optimize high-quality care for patients, communities, and populations.
Objectives:
- Student applies knowledge of social and structural drivers of health.
- Student adapts performance to various healthcare teams, delivery settings, and systems.
- Student collaborates in transitions and coordination of care.
- Student identifies the risks and benefits of using current and emerging technologies in patient care.
- Student identifies patient safety concerns, systems issues, and opportunities for quality improvement.
- Student describes health policy and the financial context of healthcare.
- Student applies knowledge of the local population and community health needs, disparities, and resources.
-
Utilizes recognized mechanisms to reduce health disparities and advance health equity in patients, communities, and healthcare systems.
Objectives:
- Student integrates patient, family, and caregiver needs, values, preferences, experiences, and social context into patient care.
- Student identifies personal biases and strategies to mitigate their effects.
- Student demonstrates social responsibility and a commitment to service.
- Student identifies individual and structural factors that impact health and wellness.
-
Demonstrates intellectual curiosity and the skills necessary to create new knowledge, devise plans for implementation of ethical research and communicate of findings.
Objectives:
- Student demonstrates knowledge of the scientific principles, research design, and data interpretation underlying basic, clinical, and translational research.
- Student gathers and analyzes existing literature in a field of inquiry and formulates a research question and hypothesis.
- Student describes appropriate research methods to answer an investigative question.
- Student demonstrates the skills to perform ethical research.
- Student communicates knowledge obtained from scientific inquiry clearly and accurately.
Admissions
A working group of the Medical Student Subcommittee has created a new policy on admissions. Members of the working group included admissions experts from both schools.
Applicants will apply to one school with a single set of admissions requirements (Medical College Admission Test, prerequisite courses, experiential preparation, and letters of recommendation). Applicants will have the opportunity to apply to the Newark and New Brunswick campuses or to a single campus. All applicants will complete the multiple mini interview and a traditional one-on-one interview.
The admissions process includes:
- Standard MD Applicant Process*, which involves:
- One future Rutgers School of Medicine
- One Admissions Committee
- One set of medical school admissions requirements
- One American Medical College Application Service submission to one school
- One secondary application
- One Interview Committee
- Taking best practices from each of the current admissions approaches
- Single Executive Admissions Committee
*Pathway program admissions will be overseen by the single admissions committee. The campuses can retain the unique aspects of their respective pathway programs.
Bylaws
Accordion Content
-
Secton I.1 Mission/Vision/Values
(a) Mission: We develop physicians and scientists to advance health through compassionate care, innovative research, and transformative education, fostering health equity and engagement across diverse communities.
(b) Vision: To be a national leader in academic medicine and health equity by reimagining medical education, discovery, patient care, and service to the community to improve outcomes for all.
(c) Values: Excellence, Integrity, Dignity, Collaboration, Belonging
Section I.2
Nothing in these Bylaws shall contravene any provision of any applicable university policies and procedures, Rutgers collectively negotiated agreements, or applicable laws and regulations. These Bylaws are constructed to recognize and implement the principle of shared governance of RSM as recognized by the University.
-
Section II.1 Definitions
(a) Faculty: The Faculty of Rutgers School of Medicine (RSM) shall consist of all individuals who have a faculty appointment.
(b) Faculty Assembly: The Faculty Assembly will consist of all faculty members who meet the following criteria: (i) are 50% or more full time equivalent, employed by RSM, (ii) have an unmodified title, and (iii) are a level of distinguished professor, professor, associate professor or assistant professor; or are an RBHS instructor or RBHS lecturer with at least one year of employment
(c) Additional members of the general faculty (The Faculty of RSM) may be appointed to the Faculty Assembly by the Faculty Council and/or the dean if they serve in a critical or significant teaching or research role or are considered for membership on a standing committee. Such appointments must be reviewed every three years.
Section II.2 Responsibilities, Authority, and Privileges of the Faculty Assembly
(a) Development and revision of the curriculum, academic calendar and overall educational program of the RSM through the actions of the Curriculum Committee.
(b) Establishment and revision of criteria for admissions, promotions, disciplinary actions and degree requirements for students of the RSM through the actions of the Admissions Committee, Curriculum Committee and Student Promotion and Progress Committee. The Faculty Assembly votes to approve the list of graduates.
(c) Participation in teaching, research, elections, committees, administrative, and/or health care delivery programs on behalf of the RSM to the extent that aligns with each faculty member’s academic rank and terms of appointment. The dean has the authority to make decisions when necessary.
(d) Recommendation of amendments to the Bylaws governing the RSM.
(e) Recommendation to the Executive Committee (Section VIII.3 Executive Committee) for goals and policies regarding professional fulfillment and belonging for faculty, staff, and students.
(f) Compliance with professionalism standards as established by the RSM in accordance with the most current Rutgers Health Statement on Professionalism in the Workplace.
Section II.3 Faculty Assembly Officers
(a) The Faculty Assembly officers shall consist of (i) Two co-presidents – one from each RSM campus, elected from among the four vice presidents from the previous term (ii) Four vice presidents, one basic science, one clinical from each RSM campus. (iii) Two secretaries – one from each RSM campus. All officers serve two-year terms and may serve a maximum of two consecutive terms in that specific officer position. Faculty officers can serve a maximum of five terms in a 15-year period.
(b) Officers must be members of the Faculty Assembly, excluding chairs, decanal level faculty, institute/center directors, and those who report directly to the dean.
(c) If an officer is unable to complete a term, there will be a new election.
-
Section III.1 Duties and Authority
(a) RSM is a medical school with two co-equal campuses, one in Newark, one in New Brunswick with a single dean. Under the chancellor of RBHS and the president of the university, the dean shall be the chief academic and administrative officer of the school with primary responsibility for implementing the missions of the school. The dean’s duties and powers shall include the following:
(i) Primary responsibility for the school's educational, research, clinical, and service/community engagement programs; for the development of teaching and research affiliations; for administration of the school; for promotion of the school's development and effectiveness; and for maintaining accreditation with appropriate groups or agencies;
(ii) Supervision of members of the academic and non-academic staff of the school;
(iii) Making recommendations on appointments, reappointments, and promotions of the faculty and conferral of tenure consistent with all university policies and applicable collective negotiation agreements;
(iv) Oversight of the implementation of the university’s processes for the review of the performance of individual faculty members;
(v) Oversight of the development and implementation of mentoring and career development plans and actions for individual faculty members;
(vi) Making recommendations to the chancellor of appointment, reappointment, and promotion of qualified individuals to serve as administrators of the school;
(vii) Preparation and presentation of the annual budget to the chancellor;
(viii) Review and approval of the expenditure of funds allocated to the school consistent with university policy and oversight by the chancellor;
(ix) Assignment of the school’s space;
(x) Representing the school in the collaborative work with leadership of the school’s hospital partners, and other affiliates to promote the success of the clinical enterprise and ensure their support of the academic/education mission;
(xi) Oversight of all activities related to LCME accreditation;
(xii) Leading the relationship between RSM with community and other external constituent groups;
(xiii) Submission of reports and recommendations to the chancellor, university president, and the Board of Governors concerning the operation, plans, and development of the school, as required;
(xiv) Ensuring that the teaching programs at the undergraduate medical education, graduate medical education, continuing education, and MD/PhD training provide a positive learning experience, offering high-quality and innovative educational opportunities to facilitate the transition from student to professional;
(xv) Overseeing and advancing the school's research program, ensuring its alignment with the institution’s mission, strategic goals, and compliance with applicable regulations;
(xvi) Leading fundraising activities successfully on behalf of RSM in collaboration with the chancellor and the development offices of the medical school and university;
(xvii) Fostering alumni recognition and participation in the growth of the school;
(xviii) Promoting collaborative relationships with Rutgers Health and the other Rutgers Schools to further the goal of interdisciplinary health science education, research, and patient care;
(xix) Ensuring that the school continues to be a leader working in the communities it serves, to address health and social welfare of those communities;
(xx) Leading and implementing a strategic plan; and
(xxi) Any other duties and powers appropriately granted by the RBHS chancellor or the president of the university.Section III.2 Appointment
(a) The dean shall be appointed by the chancellor. The chancellor shall select the dean from among a slate of nominees provided by a dean’s Search Committee. The chancellor shall select the majority of the search committee members from a slate elected by the RSM Faculty Assembly through a Faculty Assembly vote. The remainder of the search committee members will be appointed by the chancellor.
(b) The dean shall serve at the discretion of the chancellor.
Section III.3 Review
(a) There shall be a periodic review of the school approximately once every five years. The chancellor shall appoint a committee to conduct the review and to report its findings and recommendations to the chancellor. The chancellor shall select faculty representation from among a slate of nominees provided by the Executive Committee. The committee shall take steps to ensure that the faculty and other appropriate constituencies have the opportunity for input to the committee’s review. The faculty shall have the opportunity to review the report once completed.
Section III.4 Appointments and Delegation of Authority
(a) The dean may, with the approval of the chancellor, appoint and delegate authority and/or responsibility to such subordinate administrative officers as may be deemed necessary for effective administration. All appointees shall serve at the pleasure of the dean.
(b) The administrative officers of the RSM shall assist the dean in performing the executive functions of the school and act for the dean if and as designated.
-
Section IV.1 Departments and Centers/Institutes
(a) The school is administratively composed of two co-equal campuses with departments and decanal level centers/institutes. All references in these bylaws to centers/institutes are limited to centers/institutes wholly within the RSM. There are several departmental and center/institute structures inclusive of decanal and/or departmental level centers/institutes.
(b) The primary organizational unit of RSM is the department or decanal center/institute which consists of faculty with a unifying interest in a distinct area of knowledge or that discipline that encompasses the educational, academic discovery, and clinical needs of that field. Each department shall function under the leadership of a department chair and shall be organized in such a manner as to assure meaningful participation of the faculty in departmental governance.
(i) Each department and decanal center/institute reports directly to the dean. Each department is administered by a chair and each decanal center/institute is administered by a director who is responsible for the organization and implementation of its programs and reports to the dean.
(ii) Unless approved by the dean, all basic science and clinical faculty will receive a primary appointment to the department which best matches the discipline, or area of research focus, in which their specialty and/or sub-specialty training occurred. Secondary appointments may occur with recommendation of chairs of both departments and approval of the dean.Section IV.2 New Departments, Centers/Institutes, and Reorganization
(a) To fulfill the mission and goals of the medical school, departments and decanal centers/institutes of RSM shall be established, restructured, or removed upon recommendation of the dean with the approval of the chancellor and in accordance with any applicable Rutgers University and State of New Jersey policies and procedures.
(b) The dean will seek the advice of the Executive Committee when considering the creation or removal of a department or decanal center/institute. The Executive Committee will vote to approve whether a department, or decanal center/institute will be created, restructured, or removed.
(c) The school will follow the processes outlined in university policy and procedure.
(d) Divisions and Centers/Institutes within departments may be established, restructured, or removed with the approval of the Executive Committee and the dean, and in accordance with any applicable Rutgers University policies and procedures. Division and Departmental Center/Institute directors shall serve at the discretion of the department chair and their stewardship shall be reviewed and evaluated periodically by the department chair and reported to the dean at their discretion.
(e) Sections within the division may be established, restructured or removed when proposed by the chair with the approval of the Executive Committee and the dean. Section chiefs shall serve at the discretion of the department chair and division chief and their stewardship shall be reviewed and evaluated periodically by the department chair/division chief and reported to the dean at their discretion.
Section IV.3 Department Chairs and Decanal Center/Institute Directors
(a) There shall be a chair of each department and director of each decanal center/institute (see section IV.1 a.). The chair, center/institute director shall be responsible to the dean and shall have the appropriate authority for carrying out their respective duties, subject to their reporting line to the dean. The chair, center/institute director shall administer the affairs of the department or center/institute in consultation with its faculty. Appointment as a chair of a department is dependent on the maintenance of a faculty appointment in that department.
(b) The chair’s, decanal center or institute director’s responsibilities shall include the following:
(i) Establishment of annual goals and objectives, with delegation of these duties as appropriate;
(ii) Development and operation of departmental or decanal center/institute programs, including but not limited to, the financial management of the department or decanal center/institute;
(iii) Supervision of departmental or decanal center/institute faculty and staff;
(iv) Conduct objective evaluations of faculty and staff consistent with RBHS and University policies and procedures, and any applicable collective negotiations agreements;
(v) Continuous evaluation of the educational, research, service and, where appropriate, patient care programs, faculty and staff performance, and administrative processes of the department or decanal center/institute and making appropriate recommendations to the dean regarding all issues of concern to the department;
(vi) Promoting mentorship for career development for individual faculty members;
(vii) Recommendation by department chairs of the appointments, reappointments, promotions, sabbaticals, unpaid leaves of absence, dismissals, and acceptance of resignations, in accordance with university policy and applicable collective negotiations agreements;
(viii) Evaluation of the department or decanal center/institute's educational, research, service and, where appropriate, patient care programs;
(ix) Oversight of clinical matters in coordination with clinical affiliate leadership
(x) Educational and research services offered by the department or decanal center/institute; and recruitment, development, and retention of outstanding clinicians and clinical and academic leaders ensuring that the necessary range of high-quality services is available to meet the needs if applicable;
(xi) Preparation and submission of an annual report to the dean regarding instructional activities, professional activities, research performance, scholarly publications and other scholarly works, clinical activities, service accomplishments, performance and progress of departmental or decanal center/institute faculty and staff;
(xii) Convening the necessary advisory departmental or decanal center/institute committees in accordance with Rutgers policies and procedures and RBHS guidelines;
(xiii) Maintenance of fully accredited, high-quality residency and fellowship programs with effective supervision of trainees if applicable;
(xiv) Representation of all department or decanal center/institute members in matters concerning the department or decanal center/institute within the clinical affiliates, and representation of the clinical affiliate perspectives to the faculty and school as needed if applicable;
(xv) Ensuring the quality of educational programs as clinical affiliates in coordination with clinical affiliate leadership;
(xvi) Service on clinical affiliate committees as requested if applicable; and
(xvii) Additional duties as assigned by the dean.(c) Appointment of Department Chairs and Decanal Center/Institute Directors.
(i) There shall be a chair for each department and director of each decanal center/institute appointed by the dean with the approval of the chancellor, in accordance with the procedures given below. The term of appointment shall be for five years and is renewable upon the recommendation of the dean and approval of the chancellor.
(ii) The process for the selection of department chairs and decanal center/institute directors shall involve the formation of a Search Committee. The dean shall solicit nominations from the Faculty Assembly. The Search Committee will be appointed and charged by the dean, with suitable consultation, to ensure appropriate representation from the relevant domain areas across the academic community. At least one member of the Search Committee will be from the department or decanal center/institute for which the chair or decanal center/institute director shall be selected. The Search Committee will actively engage stakeholders during the search process through a variety of means, to make certain that all interested parties can share their perspective with the committee. At the conclusion of the process, the Search Committee shall provide the dean with a list of acceptable candidates for consideration. The dean shall select the chair or decanal center/institute director for final approval by the chancellor.
(iii) All department chairs and decanal center/institute directors shall serve at the discretion of the dean. The performance of each chair and decanal center/institute director will be reviewed annually by the dean.
(iv) Once every five years or at any time during the term of a departmental chair or center/institute director, a review and evaluation of the department, decanal center/institute and of the stewardship of the chair or director may be initiated by the Dean. Process for review of chair or center/institute directors is outlined in RSM Policy and Procedures. The dean may also initiate such a review under the following circumstances: if requested by the Executive Committee or Faculty Council, or upon petition by over 50% of the departmental Faculty Assembly members.- The dean may reappoint a departmental chair or decanal center/institute director after formal consultation with the department or may declare the chair vacant. However, chairs and decanal center/institute directors serve at the discretion of the dean without regard to term or review.
- In the case of a vacancy, the dean may appoint an interim chair or decanal center/institute director after formal consultation with the members of the department or center/institute. The interim chair or decanal center/institute director shall serve at the discretion of the dean.
-
Section V.1 Regular Meetings of the Faculty Assembly
(a) The Faculty Assembly shall meet no less than three times per year. Meetings may take place in person, virtually, or in a hybrid format.
Section V.2 Special Meetings of the Faculty Assembly
(a) Special meetings of the Faculty Assembly may be called to ensure the effective discharge of the business of the school.
(b) Either of the co-presidents of the Faculty Assembly or the dean may call for a special meeting of the Faculty Assembly.
(c) 50 members of the Faculty Assembly may, by petition, cause the co-presidents of the Faculty Assembly to call a special meeting.
Section V.3 Meeting Procedures
(a) Meetings shall be presided over by the co-presidents of the Faculty Assembly. In the co-presidents' absence, a vice president shall preside alternating by campus location.
(b) The presiding officer will be responsible for setting the agenda. The agenda will be circulated at least seven calendar days in advance of the meeting.
(c) Items requiring a vote will be discussed at faculty meetings, but voting will be conducted electronically.
(d) For votes of the Faculty Assembly to recommend revisions to the bylaws, two-thirds of Faculty Assembly members constitute a quorum and a majority of votes determines the outcome, and greater than 50% of departments must be represented by two or more faculty. For all other votes, a simple majority of votes determines the outcome.
-
Section VI.1 Charge
(a) The Faculty Council serves as a liaison between the faculty and administration of the school on issues significant to the faculty.
(b) The Faculty Council shall receive reports from all the standing committees and shall provide recommendations and advice.
(c) The Faculty Council may propose changes to policies of the standing committees which must be approved by the standing committee and Executive Committee.
(d) The Faculty Council may propose changes to the bylaws of the RSM which would be referred to the Faculty Assembly for approval.
(e) The Faculty Council may propose policies pertaining to all academic matters which come under the jurisdiction of the general faculty and Faculty Assembly. These policies would also require approval of the Executive Committee.
(f) The co-presidents of the Faculty Assembly, with the approval of the Faculty Council, may appoint ad hoc committees of the Faculty Council.
Section VI.2 Officers
(a) The Faculty Council will be chaired by the co-presidents of the Faculty Assembly. The co-presidents will preside at all meetings of the Faculty Council. In the co-presidents’ absence, a vice president shall preside.
Section VI.3 Membership and Terms of Service
(a) Membership of the Faculty Council:
(i) Three department chairs from each campus, two clinical and one basic science, to be elected by the department chairs. Both surgical and non-surgical clinical departments should be represented (surgical departments include Anesthesia, Neurosurgery, Ob Gyn, Orthopedic surgery, OHNS, Ophthalmology, and nonsurgical include Emergency Medicine, Family Medicine, Medicine, Neurology, Pathology, Pediatrics, PMNR, Psychiatry, Radiology and Radiation Oncology).
(ii) Representatives from each department on each campus depending on department size, elected by the department. Each department will have one representative for every 30 faculty assembly members, up to a maximum of five representatives.
(iii) Three at-large faculty members from each campus, one basic science and two clinical, elected by the Faculty Assembly annually. Eligibility criteria: Member of the Faculty Assembly above rank of instructor.
(iv) Medical student government president from each campus, without vote.
(v) Two representatives from the dean’s office, one from each campus, designated by the dean.
(vi) The co-presidents of the Faculty Assembly, with the approval of the Faculty Council, may appoint ex officio non-voting members to the Faculty Council.(b) Terms - The terms of service of the Faculty Council will begin September 1 and end August 31. A Faculty Council representative will serve a term of two years and may not serve for more than two consecutive terms. Terms will be staggered by electing one-half of the Faculty Council representatives each year.
Section VI.4 Meetings
(a) Regular Faculty Council meetings will be held monthly, on a day and time decided by the Faculty Council. Meetings may be cancelled by the officers, with the exception that meetings must be held at least 10 times a year. Special meetings may be called by any five voting members of the Faculty Council.
Section VI.5 Vacancies
(a) The voting faculty shall elect a replacement to complete an unexpired term of an elected member if greater than one calendar year.
-
Section VII.1 Eligibility to Serve on Standing Committees
(a) Membership. All members of the Faculty Assembly of RSM in good standing are eligible for election or appointment to standing committees as voting members. Membership on standing committees shall be comprised of elected faculty and faculty appointed by the dean. Staff may serve on committees in an advisory capacity. The faculty are eligible for appointment to subcommittees and/or ad hoc committees. Standing committees shall have equal representation from each campus. Elections and appointments shall assure equal representation from each campus.
(b) The length of term and number of terms for the election or appointment of standing committee members are noted in Article VIII. Members may be appointed by the dean to successive terms or elected to successive terms by their peers during school elections unless otherwise specified by the committee. Emeritus committee members may serve in advisory roles, as requested by the chair.
Section VII.2 Nominations, Elections and Appointments
(a) Nominations, elections, and appointments for standing committee membership will be administered by the Advisory Board on Committee Nominations. The Advisory Board on Committee Nominations is responsible for:
(i) Preparing a slate of candidates who will stand for election to the standing committees; and
(ii) Reviewing and advising the dean on proposed appointments to the standing committees.(b) The Advisory Board on Committee Nominations may also identify and recruit faculty members for additional elected or appointed positions whenever Faculty Council input into those positions is desired or appropriate.
(c) The Advisory Board on Committee Nominations will endeavor to include representation of a diverse rank of professional experiences and viewpoints in preparing a slate of candidates who will stand for election to the standing committees. Nominations may be solicited via written or electronic correspondence, or in person. The willingness of nominated candidates to serve in positions will be confirmed prior to elections.
(d) The composition of the Advisory Board on Committee Nominations will include balanced membership representing each campus. Membership will consist of:
(i) The Faculty Council co-presidents
(ii) The Faculty Council vice presidents
(iii) The Faculty Council co-secretaries
(iv) Dean’s senior leadership group(e) This Advisory Board on Committee Nominations should meet at least once per academic year.
(f) After preparation of a slate of candidates for election, Faculty Assembly members will have the opportunity to nominate or self-nominate at a Faculty Assembly meeting. Elections will be administered electronically by the Advisory Board on Committee Nominations with quorum defined as 25% of the Faculty Assembly from each campus.
Section VII.3 New Standing Committees
(a) Standing committees shall be created, altered, or abolished by amendment of these Bylaws.
Section VII.4 Special Committees
(a) Special committees (e.g., ad hoc committees and task forces) may be appointed by the dean. Such committees or task forces should have a specific charge and an expected deadline for completion of their assigned task. Unless they have a task that only affects a narrow constituency, ad hoc committees, task forces, or special committees should have representation from both campuses and should have broad representation from within the school selected from diverse departments, and type, and rank of faculty members.
-
Section VIII.1 Admissions Committee
(a) Charge and authority: The Admissions Committee shall:
(i) Develop, review, and establish policies regarding the prerequisites, admissions standards, and admissions procedures for student application and acceptance into the RSM, subject to the approval of the Executive Committee.
(ii) Evaluate candidates for admission to the MD and MD-PhD programs of the RSM.
(iii) Recommend qualified applicants to be offered admission to the RSM. The final responsibility for accepting students to the school rests with the Executive Admissions Committee.
(iv) The Executive Admissions Committee is empowered to establish subcommittees from its membership as it deems necessary to carry out its functions.(b) Membership: The Admissions Committee consists of the following 78 voting members:
(i) 60 faculty, 30 are from the Newark campus and 30 are from the New Brunswick campus. Fifteen shall be elected by the Faculty Assembly and 15 appointed by the dean at each campus. Faculty members will serve three-year terms, with no limit to how many terms a member can serve and no departmental restrictions.
(ii) 18 students of RSM, nine from the Newark campus and nine from the New Brunswick campus. Of these nine students from each campus, three will be from M2, M3, and M4 classes, each. Students will be selected by the Student Council and appointed by the faculty of the Executive Admissions Committee.(c) Officers: There will be one chair and one vice chair over both the Executive Admissions Committee and the Admissions Committee. The chair and vice chair roles will come from both campuses and the roles will switch annually. The chair and vice chair will be appointed by the dean.
(d) The Executive Admissions Committee of the Admissions Committee
(i) Membership of the Executive Admissions Committee will consist of the following 30 voting members:- 24 faculty, of which 12 are from the Newark campus and 12 are from the New Brunswick campus. Members will be selected from the Admissions Committee and appointed by the chair of the Executive Admissions Committee.
- Six students of RSM, three are from the Newark campus and three from the New Brunswick campus. Members will be selected from the Admissions Committee and appointed by the chair of the Executive Admissions Committee.
- Ex-officio non-voting membership could include representation from the MD/PhD program.
- The chair of the Executive Admissions Committee will be the chair of the Admissions Committee
(e) Meeting frequency: Meetings of the Admissions Committee are held at least 12 times over the 12-month academic year, with the goal of occurring at least monthly. The chairs may designate additional meeting dates.
(f) Quorum: The presence of 50% of members of the Executive Admissions Committee shall constitute quorum at any meeting of the Executive Admissions Committee. The presence of 50% of members of the Admissions Committee from each campus, including 2/3 of those who interviewed applicants on a given agenda, shall constitute a quorum at any meeting of the Admissions Committee.
(g) Reports: Annually, the Admissions Committee will report a written summary of their past year's work and plans for changes to policies and upcoming year's work to the Faculty Council and the Executive Committee.
Section VIII.2 Curriculum Committee
(a) Charge and authority: The Curriculum Committee is responsible for the overall design, management, integration, evaluation, and enhancement of a coherent and coordinated medical curriculum.
(b) Membership: The Curriculum Committee will consist of 20 faculty members, 10 from each campus. From each campus, five shall be elected by the Faculty Assembly and five shall be appointed by the dean. There will be representation from basic and clinical sciences. Each elected member will serve a three-year term, except if serving in a leadership role, in which case, terms may be extended. There will be six student members (three from each campus) from M2, M3 and M4 years. All education and student affairs deans and university librarians serve as ex-officio, non-voting members. Administrative support staff from the Office of Education may be appointed by the dean as non-voting members.
(c) Officers: The Curriculum Committee chair will be appointed by the dean. The Curriculum Committee will elect 2 vice chairs, one basic science and one clinical, every two years from the committee membership. The immediate past-chair will remain on the committee for two years. Committee members cannot hold administrative (decanal and chair) roles.
(d) Meetings: Regular meetings shall be held at least bi-monthly or as deemed necessary by the chair.
(e) Quorum: A meeting quorum is defined as at least 50% of the members of the Curriculum Committee from each campus.
(f) Reports: The Curriculum Committee actions shall be reported in summary fashion to the Faculty Council and Executive Committee following each regular meeting. Occasionally, substantive changes in the degree requirements may be necessary, either at the recommendation of accrediting bodies or as initiated by the faculty. The Curriculum Committee will bring recommendations for major curricular change to the dean, Executive Committee and the Faculty Council for comprehensive input from the dean and the faculty. The final authority for the curriculum lies with the Curriculum Committee.
(g) Subcommittees: The committee will have subcommittees responsible for pre-clinical and clinical curricula. The Curriculum Committee vice chairs will chair these subcommittees. These subcommittee meetings may be held more frequently, at least once before each regular committee meeting.
Section VIII.3 Executive Committee
(a) Charge and authority: The Executive Committee of the Faculty will:
(i) Advise the dean on various policies and procedures concerning the school and university
(ii) Facilitate communication among leadership of the academic units of the school
(iii) Approve policies and procedures of the school’s standing committees pertaining to the school’s academic programs, including specific authority to:- Approve major changes in educational program policy
- Approve all Distinction programs
- Approve all departmental changes in compliance with university policy, e.g., new departments, dissolution of departments, adding divisions, etc. with the final approval consistent with Rutgers University Policy.
(b) Membership: The Executive Committee of the faculty will be chaired by the dean and consist of:
(i) All academic department chairs
(ii) School decanal institute and center directors
(iii) The officers of the Faculty Assembly (two presidents, four vice presidents, two secretaries)
(iv) The associate and vice deans of the school who serve in an ex officio without vote
(v) Other faculty as determined by the dean(c) Terms: An individual serves on the Executive Committee of the faculty while holding his/her leadership position.
(d) Officers: The dean or the dean’s representative shall serve as chairperson of the Executive Committee.
(e) Meetings: The Executive Committee shall meet monthly and at other times upon call of the dean or the dean’s representative.
(i) The dean, or the dean’s representative of the Executive Committee shall preside.
(ii) Minutes of all meetings shall be kept for future use of the Executive Committee and the dean.
(iii) The agenda for Executive Committee meetings shall be prepared by the dean or dean’s representative and shall be distributed to the members before each meeting. Agenda items may be submitted to the dean by members of the Executive Committee.(f) Quorum: The presence of 50% of the members of the Executive Committee from each campus and the presence of 50% of the Department Chairs shall constitute a quorum at any meeting of the Committee.
Section VIII.4 Advisory Committee on Appointments and Promotions
(a) Charge: The Advisory Committee on Appointments and Promotions shall have the responsibility of advising the dean as to appointments, reappointments of tenure-track faculty, promotions, granting of tenure, changes in track, sabbatical. The dean shall obtain the advice of this Committee in these matters. All matters of faculty appointment and promotion shall be in accordance with “RBHS Policies and Guidelines Governing Appointments, Promotions, and Professional Activities of the Faculty,” University policy and procedure, and collective negotiation agreements as applicable.
(b) Membership: The Advisory Committee on Appointments and Promotions shall consist of 24 members, 12 from each campus. Six shall be elected by the Faculty Assembly and six appointed by the dean at each campus and the final composition of the committee will be six basic science and six clinical faculty from each campus. The deans for Faculty Affairs shall serve ex officio without vote. All members must be professors or distinguished professors, at least eight of the members must be tenured, and no more than two members may be from the same department. No more than two members may be a chair of a department. The term of office shall be three years, with staggered terms. No member standing shall serve more than two consecutive terms. Ad hoc committee members may be appointed by the dean in order to meet quorum for decisions concerning tenure track faculty.
(c) Officers: The members shall elect a chair from among the members.
(d) Meetings: Meetings shall be convened to comply with the institutional deadlines.
(e) Quorum: A quorum shall be 10 members, including five members from each campus and the chair or a designated alternate from the members of the committee. For decisions concerning tenure track faculty, only tenured members may vote, and there must be a minimum of six such members.
(f) Reports: All departmental actions presented to the Advisory Committee on Appointments and Promotions must include a report of the results of the deliberations of the advisory committee of the department.
Section VIII.5 Research Committee
(a) Charge: The goal of this committee is to enhance the research enterprise by disseminating research-related information to faculty, by facilitating communication between investigators and administration, and by advocating for optimal practices and conditions that foster research productivity. The committee encourages innovation, stimulates new investigative endeavors, fosters interdisciplinary and transdisciplinary approaches, and provides counsel on the identification and wide use of institutional resources. The committee shall make recommendations to the dean and to the Faculty Council regarding implementation of efficient research programs.
(b) Membership: The Research Committee shall consist of 16 members, 8 from each campus. From each campus, four shall be selected by the Faculty Council and four appointed by the dean at each campus and the final composition of the committee will be four basic science and four clinical faculty. Research deans from both campuses will serve as ex-officio members.
(c) Terms: Members will serve three-year terms.
(d) Meetings: The committee will meet at least ten times per year.
(e) Reports: Annually, the Research Committee will report a written summary of their past year's work and plans for changes to policies and upcoming year's work to the Faculty Council and the Executive Committee.
Section VIII.6 Student Promotion and Progress Committee
(a) Charge and authority:
(i) This Committee shall have the responsibility of monitoring and designating the academic status of all students in the M.D. and M.D-PhD curriculum of RSM, and of formulating the Academic Rules and Regulations, which provide the guidelines for promotion and awarding of degrees.
(ii) Actions of the Student Promotion and Progress Committee may include, but are not limited to, the following:- Recommendation to the Faculty Assembly the candidates for the M.D. degree
- Establish policies and procedures pertaining to student promotion and progress.
- Determination that medical students have satisfactorily met the requirements of each academic year in the M.D. curriculum and all joint degree programs
- Decisions on students for promotion to the next academic year
- Decisions on appeals of non-passing grades and remediation decisions made by courses and clerkships
- Mandate for reduced course load, modified curricula, or other forms of extending a medical student’s curriculum due to academic difficulties
- Placement of students on Academic Warning or Academic Suspension
- Decisions on requested leaves of absence for students in academic difficulty
- Decisions on appeals for an exception to the application of the Academic Rules & Regulations (AR&R)
- Dismissal of students
- Establish standards for Satisfactory Academic Progress and consider related appeals
(b) Membership: The committee will be comprised of:
(i) 18 faculty, nine from each campus. From each campus, four are appointed by the dean, four are elected by the Faculty Assembly, and one MD-PhD core faculty is appointed by the director of the MD-PhD program. Faculty will serve three-year, staggered terms with reappointments possible.
(ii) The deans for education, student affairs, and the registrar shall serve ex officio without vote.(c) Officers:
(i) Chair: One member with at least two years of service on the committee shall be designated the chair by the dean and will serve as the presiding officer. The chair’s responsibilities are to set the agenda, assign duties and responsibilities to the committee members, report to the Executive Committee and dean on a regular basis. The chair will serve for three years and may be reappointed for an additional three years.
(ii) Two Vice-Chairs: The committee will elect two faculty members, one from each campus to serve as vice chairs. The vice chair’s responsibilities include assisting the chair and serving as the chair when the chair is unavailable. The vice chair will serve for up to three years and may be reappointed for an additional three years.(d) Meetings: The committee will meet monthly.
(e) Reports:
(i) The committee shall provide a summary report annually to the Executive Committee.
(ii) The committee shall deliver reports to the Faculty Council on a semi-annual basis.(f) The committee will decide on the formation of subcommittees or ad hoc committees.
(g) Quorum: 50% of members from each campus will define the quorum. Voting on an item will pass with a majority.
-
Section IX.1 Approval Process
(a) In order for an amendment of the Bylaws to be considered, the dean, Executive Committee, or the Faculty Council shall have the right to propose the amendment at a meeting of the Faculty Council where there is a quorum across the two campuses for discussion. The proposed amendment and justification will be discussed at a meeting of the Faculty Assembly. The Faculty Assembly will vote on the proposed amendment after the meeting. The vote must be open for a minimum of two weeks. A quorum is 2/3 of Faculty Assembly will constitute quorum. Voting on an amendment will pass with a majority.
(b) All amendments to these Bylaws must be presented to the dean and chancellor for approval.
(c) These Bylaws shall take effect approved by the dean and the chancellor.
Section IX.2 Regular Review of the Bylaws
(a) A full review of these bylaws should be conducted at least every five years. The dean shall appoint a committee and chair to examine the Bylaws and propose such revisions as seem desirable.
(b) Any proposed revisions will be subject to the approval process above.
-
Integration Executive Committee Approval April 14, 2025
Approved June 25, 2025
Leadership
Officers of the future Rutgers School of Medicine Faculty Assembly will serve as the inaugural leadership of the combined medical schools. The faculty assembly will function as an important forum for faculty voice, representation, and collaboration as we continue to build our shared culture and academic identity.
Co-Presidents
Sara Morelli, MD, PhD
Professor, Obstetrics, Gynecology and Reproductive Health, NJMS
Nell Maloney Patel, MD
Professor, Surgery, RWJMS
Co-Vice Presidents, Basic Science
Nan Gao, PhD
Professor, Pharmacology, Physiology and Neuroscience, NJMS
M. Chiara Manzini, PhD
Associate Professor, Neuroscience and Cell Biology, RWJMS
Co-Vice Presidents, Clinical
Anne Sutherland, MD
Associate Professor, Medicine, NJMS
Geza K. Kiss, MD
Professor, Anesthesiology and Perioperative Medicine, RWJMS
Co-Secretaries
Samantha Bell, PhD
Assistant Professor, Microbiology, Biochemistry & Molecular Genetics, NJMS
Steve Khalil, MD
Associate Professor, Medicine, RWJMS
Committees
Accordion Content
-
Co-chairs: Deans Robert L. Johnson and Amy P. Murtha
- Consists of designated leaders representing each of the mission areas from both NJMS and RWJMS.
- Provides strategic oversight of the integration planning process, addresses emergent questions and areas of concern, and ensures successful completion of the various tasks associated with the integration.
- Rutgers Office of Organizational Leadership will provide this committee with consultative support regarding the integration planning process.
Members
- Maria Soto-Greene, NJMS
- Carol Terregino, RWJMS
- Céline Gélinas, RWJMS
- William C. Gause, NJMS
- Ana M. Natale-Pereira, NJMS
- Shawna Hudson, RWJMS
- Beth Salamon, RWJMS
- LaCarla Donaldson, NJMS
- Justin Sambol, NJMS
- Keith Lewis, RWJMS
- Michael J. Petti, NJMS
- Carla Hailey Penn, RWJMS
-
Co-chairs: Carol Terregino and Maria Soto-Greene
Organized around LCME domains/standards, with faculty, staff, and student representatives from both NJMS and RWJMS:
- Governance and Administration
- Academic Environment
- Faculty
- Curriculum
- Medical Students
Committee Details and Membership
- Members in subcommittees will include a co-chair and vice chair from each school, in addition to faculty, staff and students.
- Chairs and vice-chairs of each subcommittee will serve on the LCME Self Study Committee.
- The LCME Self Study Committee will report to the Integration Executive Committee.
- The charge will be to engage in the work associated with the completion of the LCME self-study process.
- ECG will provide this committee with project management support.
Members
Governance and Administration
- Shawna V. Hudson, RWJMS (Co-Chair)
- Marc Klapholz, NJMS (Co-Chair)
- Lisa N. Gittens-Williams, NJMS (Co-Vice Chair)
- Keith Lewis, RWJMS (Co-Vice Chair)
- Renee Riggs-Fiesseler, RWJMS
- Christine M. Gerula, NJMS
- Utz Herbig, NJMS
- Nina E. Glass, NJMS
- Ram Mani, RWJMS
- Nell Maloney Patel, RWJMS
- Novneet Sahu, NJMS
- Alfred F. Tallia, RWJMS
Academic Environment
- Celine Gelinas, RWJMS (Chair)
- Ana Natale-Pereira, NJMS (Chair)
- Phil Messica, RWJMS (Vice Chair)
- David Roe, NJMS (Vice Chair)
- Charletta Ayers, RWJMS
- Manasa Ayyala, NJMS
- Iris Herrera, NJMS
- Eric Jahn, RWJMS
- Franz Smith, NJMS
- Pat Whitley Williams, RWJMS
- Susannah Wise, RWJMS
Faculty Subcommittee
- Pat O'Connor, NJMS (Chair)
- Archana Pradhan, RWJMS (Chair)
- Diane Calello, NJMS (Vice Chair)
- Rhonda Smith, RWJMS (Vice Chair)
- Paul Copeland, RWJMS
- Michael Kelly, RWJMS
- Maral Mouradian, RWJMS
- Anupama Nehra, NJMS
- Amariliz Rivera-Medina, NJMS
- Michael Steinberg, RWJMS
- Harsh Sule, NJMS
- Andrew Thomas, NJMS
Curriculum Subcommittee
- Liesel Copeland, RWJMS (Chair)
- Christin Traba, NJMS (Chair)
- Sophia Chen, NJMS (Vice Chair)
- Sarang Kim, RWJMS (Vice Chair)
- Sara Dunn, NJMS
- Alla Fayngersh, NJMS
- Diana Glendinning, RWJMS
- Malvika Kaul, RWJMS
- Robert Lebeau, RWJMS
- Archana Pradhan, RWJMS
- Kei Wong, NJMS
- Ian Whitehead, NJMS
Medical Student Subcommittee
- James Hill, NJMS (Chair)
- Daniel Mehan, RWJMS (Chair)
- Sonia Garcia Laumbach, RWJMS (Vice Chair)
- Michael Shapiro, NJMS (Vice Chair)
- Luis Alzate-Duque, NJMS
- Liesel Copeland, RWJMS
- Kristen Coppola, RWJMS
- Sharon Gonzales, NJMS
- Shilpa Pai, RWJMS
- Hanin Rashid, RWJMS
- Mercedes Rivero, NJMS
- Cheryl Slaughter-Hurst, NJMS
-
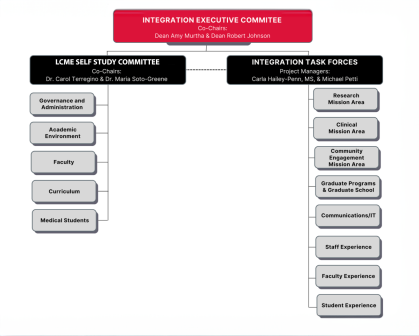
Task Forces
Accordion Content
-
Each task force is co-chaired by individuals from both NJMS and RWJMS. Carla Hailey Penn and Michael Petti provide project management support to the task forces to ensure consistency of goals, deliverables, and timelines.
Task forces are organized around cross-cutting issues of importance. The Integration Advisory Committee relies on these task forces to provide meaningful input to the LCME self-study process and to other important areas (additional task force groups will be added as needs arise):
- MD and PhD Programs
- Medical Student Activities
- Governance
- Primary Care
Composition and Responsibilities
Each task force has equal representation from each campus. They are populated by faculty, staff, and students. A peer- or self-nominated slate of candidates is presented to leadership for selection. Leadership then selects the final roster for task forces.
Role of Task Forces
- Informing integration leadership on key issues related to them/their area
- Reviewing and providing feedback to the Integration Advisory Committee and subcommittees
- Setting agenda for their work
- Identifying areas for reconciliation
- Sharing existing practices
- Identifying best practices
- Considering pathways for areas for reconciliation
Co-Leaders
MD and PhD Programs
- William Hu, RWJMS
- Michael Rallo, RWJMS
- Amariliz Rivera, NJMS
- Arwan Sawhney, NJMS
Medical Student Activities
- Miri Goodman, RWJMS
- Pia Kapoor, NJMS
- Mercedes Padilla-Register, NJMS
- Kusum Punjabi, RWJMS
Governance
- Sree Gogineni, RWJMS
- Sonia Laumbach, RWJMS
- James Takahashi, NJMS
- Waez Umer, NJMS
Primary Care
- Joyce Afran, RWJMS
- Ethan Halm, RWJMS
- Rachel Rosenberg, NJMS
- Alan Tso, NJMS
-
Co-Leaders
Alumni Task Force
- Kristen Echanique, NJMS
- George Heinrich, NJMS
- Elias Iliadis, RWJMS
- Paul Weber, RWJMS
Clinical/Health Service Research Task Force
- Ping-hsen Chen, NJMS
- Mirela Feurdean, NJMS
- Shawna Hudson, RWJMS
- Reynold Panettieri, RWJMS
Communications Task Force
- Natalie Colimon-Fitzgerald, NJMS
- Lauren Marshall, RWJMS
- Mercedes Rivero, NJMS
- Steven Wen, RWJMS
Faculty Promotion Improvement Task Force
- Andrew Berman, NJMS
- Salma Jabbour, RWJMS
- Manuel Jimenez, RWJMS
- Debra Pittman, NJMS
Faculty Recruitment Task Force
- Ibiyonu Lawrence, RWJMS
- Joshua Lubin, NJMS
- Kameswari Maganti, RWJMS
- Yu-Lan Mary Ying, NJMS
Global Health Task Force
- Rajita Bhavaraju, NJMS
- Karen WeiRu Lin, RWJMS
- Richard Marlink, RWJMS
- Ziad Sifri, NJMS
Graduate Medical Education Task Force
- Christine Gerula, NJMS
- Michael Kelly, RWJMS
- Sara Lubitz, RWJMS
- Jared Walsh, NJMS
Medical Student Research Task Force
- Leela Biswas, RWJMS
- Todd Mowery, RWJMS
- Arman Sawhney, NJMS
- Samantha Weber, NJMS
-
Co-Leaders
Clinical Task Force
- James Guarrera, NJMS
- Juana Hutchinson-Colas, RWJMS
- Manish Patel, RWJMS
- Kristin Wong, NJMS
Communications and IT Task Force
- Maged Mohamed, RWJMS
- Beth Salamon, RWJMS
- Courtney Terry, NJMS
- Alfonso Waller, NJMS
Community Task Force
- Damali Campbell-Oparaji, NJMS
- Michelle Dalla Piazza, NJMS
- Susan Giordano, RWJMS
- Eric Jahn, RWJMS
Faculty Task Force
- Andrew Berman, NJMS
- Cheryl Dreyfus, RWJMS
- Ashley Wackym, RWJMS
- Yu-lan Mary Ying, NJMS
Grad School Task Force
- John Chan, NJMS
- Carol Lutz, NJMS
- Kathy Scotto, RWJMS
- Nancy Walworth, RWJMS
Research Task Force
- Marty Blazer, RWJMS
- William Gause, NJMS
- Amariliz Rivera-Medina, NJMS
- Derek Sant'Angelo, RWJMS
Staff Task Force
- Natalie Colimon-Fitzgerald, NJMS
- Francesca Escaleira, NJMS
- Amy Smith, RWJMS
- Roger Thornton, RWJMS
Student Task Force
- Monica Hanani, NJMS
- Isaac Huang, RWJMS
- Brooke Phillips, RWJMS
- Samantha Weber-Fishkin, NJMS
Potential Benefits
An integrated model of medical education will position the future Rutgers School of Medicine as one of the leading public medical schools in the country and create an unparalleled hub of biomedical and health sciences education, research, and clinical care.
When complete, the integration envisions a medical school that enjoys a national reputation greater than the sum of its parts, amplifying Rutgers University’s role as a leader in twenty-first century medical education.
Further potential benefits to an integration include:
-
Closer collaboration on the educational mission offers a broader scope and scale of teaching talent, learning content, and clinical experiences that will benefit educators and learners. The future Rutgers School of Medicine will expand student opportunities, providing innovative experiences on both campuses.
-
Leveraging our tremendous capacity as an integrated medical school will more accurately reflect our growing impact on clinical, translational, and basic biomedical research placing Rutgers at the forefront of the innovation economy attracting more federal and industry funding.
- Elevation in rankings – The impact of an integrated medical school on research rankings is substantial, whether looking at the ranking of individual departments or the medical school overall, and across all types of funding (e.g., federal and state funding among others), and this impacts other ranking systems (e.g., U.S. News & World Report). For example, our federal fiscal year 2021 National Institutes of Health (NIH) funding institutional rankings among 143 US medical schools are:
- Robert Wood Johnson Medical School (RWJMS) at #62 with $68 million.
- New Jersey Medical School (NJMS) at #74 with $51 million.
- Combined RWJMS/NJMS at #47 with $119 million.
- The sum is greater than the parts – Combining complementary strengths, expertise, and resources from both schools will make the integrated medical school more competitive for external research and training grants. Similarly, a larger Rutgers-oriented patient base will make us more competitive for clinical trials.
- Attracting and keeping talent – An enhanced reputation and national prominence will help to attract and retain the best research faculty and trainees.
- Elevation in rankings – The impact of an integrated medical school on research rankings is substantial, whether looking at the ranking of individual departments or the medical school overall, and across all types of funding (e.g., federal and state funding among others), and this impacts other ranking systems (e.g., U.S. News & World Report). For example, our federal fiscal year 2021 National Institutes of Health (NIH) funding institutional rankings among 143 US medical schools are:
-
A single medical school has the potential to expand our portfolio of tertiary and quaternary services and launch new services to a wider patient base this platform will help us save lives, maintain health, improve outcomes and patient satisfaction, reduce health care inequities and disparities, and create competitive fellowship programs.
- Strength and stability in the market – Current populations in each city are relatively small, especially when compared with New York or Philadelphia, making it impractical to offer as wide an array of specialized services. Additionally, our current service lines are too fragile, with the departure of one faculty member often hampering the ability to continue to offer a clinical service at the involved school. An integrated medical school provides the opportunity for greater breadth, depth, and coordination of services. This will increase our ability to offer the most specialized care, establish regional and national clinical destination programs, and better compete for market share locally and regionally.
- Improved service to our communities – Increasing our ability to offer the most specialized clinical services will better serve our communities, as patients will not need to travel to New York or Philadelphia to receive them. This minimizes, if not eliminates, barriers related to inconvenience, and expense (e.g., out-of-network care is much more expensive to the patient and the state). It also helps to address health inequities, as the most needy in our communities cannot afford to make such trips and pay for such care.
- Access to clinical trials – A larger Rutgers-oriented patient base, combined with a burgeoning research ranking and reputation, will make us more competitive for clinical trials and gain access for our patients to more cutting-edge treatments, therapeutics, and procedures.
- Attracting and keeping talent – An enhanced reputation and national prominence (see below) will help to attract and retain the best clinical faculty and trainees.
-
An integrated medical school strongly identified with Rutgers University has the potential to broaden the recognition of the excellent medical education programs and growing research portfolios than each school has individually.
- Connection to Rutgers brand – Potential faculty and students and the public may not necessarily associate NJMS and RWJMS with Rutgers. An integrated medical school provides the opportunity to tie more closely to and benefit from the stronger, nationally recognized Rutgers brand.
- Alignment with more common medical school organizational models – Excluding large university systems (e.g., University of California and University of Texas), we know of only four universities in the country that have more than one autonomous medical school (i.e., Rutgers, University of South Carolina, New York University, and University of Arizona), and at least one of those (University of Arizona) is reconsidering its organizational model.
- Advancement within the Big 10 – Each of our schools now is small, relative to other schools. In part for this reason, of the 14 Big 10 medical schools (Rutgers’ individual schools are counted separately), Rutgers now ranks only #12 (RWJMS) and #13 (NJMS), above only Michigan State University’s medical school. A combined medical school would rise to #9 in the Big 10 and be more closely comparable to the University of Iowa and Ohio State University.
- Improvement in other rankings – Published rankings are driven substantially by research, and while NJMS and RWJMS are already artificially combined in Blue Ridge’s NIH rankings, US News & World Report evaluates schools separately based on their individual accreditations (which also divides and weakens the rankings of clinical and basic science departments). It is recognized that many institutions (e.g., Columbia, Harvard, Mt. Sinai, University of Pennsylvania, and Stanford) have decided to discontinue their participation in the U.S. News & World Report medical school rankings, given concerns about how those rankings are determined. Our expectation is that the rankings will continue, as the public desires them, and we hope that U.S. News & World Report will revise its formulae to address some of the objections (as it has done for its law school rankings). At the least, they may be based more on publicly available metrics, which would make NIH funding even more important.
- More philanthropic support – Enhanced national prominence is more likely to garner philanthropic gifts to support scholarships, selective research efforts, and endowed professorships.
-
Processes and systems that inhibit faculty productivity and employee satisfaction can be streamlined.
- Increased simplicity – Structures and processes will be simpler and more straightforward, after an anticipated transition period. Examples include:
- Faculty appointment processes will not need to be repeated for someone to teach at the other campus.
- Best practices from one campus can be identified and applied in the other.
- There will be a single accreditation process.
- Rutgers Health will not need to start new centers/institutes simply to foster inter-medical school programs.
- Limiting duplication – Combining the medical schools will identify and remove redundancies in many administrative structures, mobilizing personnel and other resources to enhance the school’s primary missions.
- Increased simplicity – Structures and processes will be simpler and more straightforward, after an anticipated transition period. Examples include:
Integration Update
Dean Murtha and Dean Johnson have created a series of messages designed to inform the communities at both medical schools regarding the latest integration news and initiatives.
Latest Updates
A Message from Dean Amy P. Murtha, MD, Regarding the Inaugural RSM Faculty Assembly Officers
February 5, 2026
Dean Murtha announces the newly elected officers of the future Rutgers School of Medicine Faculty Assembly.
Integration Update: December 2025
December 9, 2025
Learn about the ongoing work of committees and task forces, as well as a new grant from the Robert Wood Johnson Foundation.
Introducing the Bylaws for the Rutgers School of Medicine
December 4, 2025
Dean Murtha and Dean Johnson share the new bylaws for the future Rutgers School of Medicine.
Integration Update: July 2025
July 29, 2025
Dean Murtha and Dean Johnson announce an opportunity to be part of the next cohort of Integration Task Forces, building on the work done so far, and exploring new focus areas.
Integration Update: April 2025
April 22, 2025
An overview of the Integration Summit, which was held on April 9, 2025
Integration Update: March 2025
March 18, 2025
Dean Murtha and Dean Johnson invite faculty, staff, and learners to register for the upcoming Integration Summit and encourage everyone to visit the future Rutgers School of Medicine integration website for ongoing updates.
Integration Update: February 2025
February 18, 2025
Dean Murtha and Dean Johnson announce the upcoming Integration Summit and encourage members of the Robert Wood Johnson Medical School and New Jersey Medical School communities to visit the future Rutgers School of Medicine integration website for ongoing updates.
Integration Update: January 2025
January 21, 2025
Dean Murtha and Dean Johnson share resources for staying up to date on the new Rutgers School of Medicine integration process.
The New Rutgers School of Medicine Releases Mission, Vision and Values Statement Focused on Advancing Health Equity
November 19, 2024
University officials say the school will become a national model aiming to curb health care disparities.
Integration Update: October 2024
October 15, 2024
Dean Murtha and Dean Johnson share an update on the thought and planning that has gone into the process of developing draft bylaws for the new Rutgers School of Medicine.
Integration Update: September 2024
September 24, 2024
Dean Murtha and Dean Johnson invite members of the community to join several new integration task forces focusing on cross-cutting areas of importance such as global health, faculty recruitment, medical student research, and more.
Integration Update: August 2024
August 19, 2024
The integration presents an exciting opportunity to create a new admissions process that draws on the strengths and expertise of both schools. Learn how both schools are working together to ensure that the new admissions process is the best it can be.
Integration Update: July 2024
July 16, 2024
Look back at key moments from our June 2024 Integration Summit, where we celebrated the progress that has been made, launched the LCME self-study for accreditation, planned the next steps in creating Rutgers School of Medicine, and more.
We’re Listening: One Year into the Rutgers School of Medicine Integration
July 15, 2024
Dean Murtha and Dean Johnson look back at a year of outreach efforts and collaboration between the RWJMS and NJMS communities in planning the merger for the new Rutgers School of Medicine.
Rutgers School of Medicine Founding Dean Appointment
July 9, 2024
Chancellor Strom announces Amy P. Murtha, MD, will serve as Founding Dean of the new Rutgers School of Medicine.
Leadership Summit Regarding the Integration of the Medical Schools: Follow-up and Link to Presentation
July 2, 2024
Update on this important leadership summit concerning the journey toward the future Rutgers School of Medicine.
Integration Update: June 2024
June 25, 2024
Dean Murtha and Dean Johnson address the ongoing work to build trust and community across the two campuses throughout the medical school integration process.
Accordion Content
-
Integration Update: May 2024
May 21, 2024
Dean Murtha and Dean Johnson share news coverage of the medical school integration and discuss recent visits with church groups, community groups, and local leaders.Integration Update: April 2024
April 23, 2024
Dean Murtha and Dean Johnson discuss several initiatives to gather input and communicate effectively with our students and communities.Integration Update: March 2024
March 19, 2024
Dean Johnson and Dean Murtha provide an update on the LCME process.Integration Update: January 2024
January 16, 2024
Dean Murtha and Dean Johnson announce the creation of a series of messages designed to inform the communities at both medical schools regarding the latest integration news and initiatives.2023
Integration Update: December 2023
December 19, 2023
Dean Johnson and Dean Murtha provide a summary of the framework that will shape the medical school integration process and invite members of the medical school communities to participate by joining a task force.Join Us for Medical Integration: Chats with the Deans
October 6, 2023
Join a virtual discussion with Dean Murtha and Dean Johnson and help us keep the momentum going as we journey toward the future as Rutgers School of Medicine.A Message from the Deans Regarding the Medical School Integration: LCME Accreditation and the Curriculum
September 26, 2023
Dean Johnson and Dean Murtha share an update about a recent webinar on LCME accreditation and the curriculum.A Message from the Deans Regarding the Medical School Integration: FAQs
September 5, 2023
Dean Murtha and Dean Johnson respond to frequently asked questions about the single accreditation process.Rutgers School of Medicine Initial Next Steps
July 21, 2023
Dean Johnson and Dean Murtha share initial next steps in the integration between the two medical schools.More Information About Medical School Integration
July 10, 2023
Following the Board of Governors' decision, Dean Murtha and Dean Johnson provide an update about the integration between the two medical schools.Rutgers Board of Governors Approves Single Medical School Accreditation
July 10, 2023
The integration of New Jersey Medical School and Robert Wood Johnson Medical School will create co-equal bodies under a single accreditation to be known as Rutgers School of Medicine.Senate Report - Envisioning the Future of Academic Medicine
January 31, 2023
Chancellor Strom announces the report on the future of academic medicine at Rutgers University has been presented to the University Senate.2022
New Website and Feedback Form for Medical School Evaluation Process
November 17, 2022
Dean Johnson, Dean Murtha, and Chancellor Strom announce the new Envisioning the Future of Academic Medicine website.Envisioning the Future of Academic Medicine: Next Steps
November 4, 2022
Chancellor Strom, RWJMS Dean Amy Murtha and NJMS Dean Robert Johnson share next steps as Rutgers Health explores the optimal level of integration and cooperation between the two medical schools.Envisioning the Future of Academic Medicine: Chancellor's Charge to the Committees
November 2022
Chancellor Brian Strom addresses the Envisioning the Future of Academic Medicine committees as they embark on the task of responding to the Rutgers University Senate's questions.Envisioning the Future of Academic Medicine at Rutgers University
September 21, 2022
Following a pause due to the pandemic, Rutgers Health will resume the process of exploring opportunities for further collaboration between New Jersey Medical School and Robert Wood Johnson Medical School.
Past Events
Integration Summit – April 9, 2025
Integration task force and committee members and department chairs from NJMS and RWJMS came together for the second Integration Summit to discuss the accreditation process, strategic pillars, and more.
Board of Governors Update – October 17, 2024
The presentation to the Board of Governors focused on our continued progression and projected pathway toward a single LCME accreditation, highlighting the positive work that has been done through the participation of joint task forces.
Watch: Virtual Town Hall – August 26, 2024
NJMS Dean Robert Johnson and RWJMS Dean Amy Murtha discuss the June 2024 launch of the LCME self-study for accreditation, share the progress of the integration committees and task forces, and provide more updates to the community.
Integration Summit – June 2024
Integration task force and committee members and department chairs from NJMS and RWJMS came together to celebrate our progress, build community and engagement, officially launch the LCME self-study for accreditation, and plan next steps.
Images from the Integration Summits
Task force and committee members and department chairs from NJMS and RWJMS came together for Integration Summits on June 26, 2024 and April 9, 2025. Click through the slideshow to view highlights from the events.




















April 2025 Integration Summit
April 2025 Integration Summit
April 2025 Integration Summit
April 2025 Integration Summit
April 2025 Integration Summit
April 2025 Integration Summit
April 2025 Integration Summit
April 2025 Integration Summit
April 2025 Integration Summit
April 2025 Integration Summit
April 2025 Integration Summit
April 2025 Integration Summit
June 2024 Integration Summit
June 2024 Integration Summit
June 2024 Integration Summit
June 2024 Integration Summit
June 2024 Integration Summit
June 2024 Integration Summit
June 2024 Integration Summit
June 2024 Integration Summit
Watch: Virtual Town Hall – September 19, 2023
Faculty, staff, students, residents, and fellows took part in a virtual discussion on September 19, 2023, about the LCME accreditation process and the medical education curriculum, with Dean Johnson, Dean Murtha, and speakers from both medical schools.
Watch: Virtual Town Hall – August 29, 2023
NJMS Dean Robert Johnson and RWJMS Dean Amy Murtha invited faculty, staff, students, residents and fellows to the first in a series of town hall discussions on August 29, 2023, to examine our individual schools' mission and vision, and respond to inquiries.
Town Hall – March 2023
Rutgers Health leadership invited members of the public to two town halls that presented an overview of the Envisioning the Future of Academic Medicine process and provided opportunities for the public to offer input.
Frequently Asked Questions
Accordion Content
Below are some frequently asked questions and answers about the medical school integration.
-
Rutgers University has two separate medical schools, each with separate accreditation. The integration is the merger of the two separate medical schools into one: the future Rutgers School of Medicine with a single accreditation from the Liaison Committee on Medical Education (LCME).
The integrated school will have comparable campuses in Newark and New Brunswick. With the future medical school, each campus will maintain its current affiliation with its principal teaching hospital and all the affiliate teaching sites.
-
Medical school integration is being pursued to create a stronger, more innovative institution that offers enhanced educational and research opportunities. By aligning and not competing, we create a hub of biomedical and health sciences education, research, and clinical care that will allow us to serve our communities better.
In the past, the two medical schools have been competitors for talent and resources. Now, we can be allies in attracting students, grants, and faculty who are pioneers in their fields.
Additionally, as the state university, we have an obligation to the residents of New Jersey to lead in transformative healthcare delivery. Through the creation of the future Rutgers School of Medicine, with comparable campuses in Newark and New Brunswick, we will have an academic healthcare delivery enterprise that will better serve all New Jersey communities.
-
An integrated model of medical education will position the future Rutgers School of Medicine as one of the leading public medical schools in the country and create an unparalleled hub of biomedical and health sciences education, research, and clinical care.
When complete, the integration envisions a medical school that enjoys a national reputation greater than the sum of its parts, amplifying Rutgers’ role as a leader in twenty-first-century medical education.
- The leveraging of our tremendous capacity as an integrated medical school will more accurately reflect our impact on clinical, translational, and basic biomedical research, will place the future school at the forefront of the innovation economy, and attract more federal and industry funding.
- Closer collaboration on the education mission offers a broader scope and scale of teaching talent, learning content, and clinical experiences that will benefit learners. The future school will expand student opportunities, providing innovative experiences on both campuses.
- It will enhance our ability to attract even more talent with reputational and ranking implications.
- A single medical school has the potential to expand our clinical portfolio of tertiary and quaternary services and launch new services to a broader patient base; this platform will help us save lives, maintain health, improve outcomes and patient satisfaction, reduce health care inequities and disparities, and create competitive fellowship programs.
Read more about the benefits of integration.
-
June 2027 is the anticipated date of accreditation of the future Rutgers School of Medicine. Summer 2028 is the time frame of the anticipated matriculation of the charter class of the future school.
-
The future Rutgers School of Medicine will have single accreditation from the LCME.
The integrated school will have comparable campuses in Newark and New Brunswick.
Growth and investment in clinical care, research, and education across the entire future Rutgers School of Medicine is the priority.
Each campus will continue its engagement and commitment to its community.
A guiding principle for creating the organizational structure of the future Rutgers School of Medicine will be one that yields enhanced collaboration and positive outcomes.
Each school would maintain its current affiliation with its principal teaching hospital as well as all the affiliate teaching sites.
The future Rutgers School of Medicine students will meet the same educational objectives and receive the same content and learning experiences. The new curriculum will increase active and engaged learning in new spaces on each of the campuses.
-
The timeline for all integration activities is based upon an anticipated granting of accreditation by the LCME in June 2027, which would allow recruitment for the charter class of the future Rutgers School of Medicine to begin in July 2028.
An Integration Executive Committee with equal representation from both schools is leading these efforts, providing ongoing strategic oversight of the integration planning process and successful completion of integration tasks. The Self Study Committee (Integration Advisory Committee), organized to fulfill the necessary LCME work, has faculty, staff, and student representatives from both schools. In addition, to elicit broad input from our school constituents as we create this new school, integration task forces have organized around cross-cutting issues of importance, such as the clinical mission, the faculty experience, and research, among others.
Read more about the process.
-
Regular updates and communications regarding the integration are provided through official channels, including email notifications, both school websites and the integration website, and town hall meetings and events. We encourage all members of the medical school communities to stay engaged and share their feedback during this transformative process.
There are also opportunities to provide feedback through surveys, town halls, committee participation, and ongoing one-on-one virtual meetups with the deans.
-
Our commitments to University Hospital in Newark and Robert Wood Johnson University Hospital in New Brunswick remain strong, and our relationship with these institutions will remain unchanged.
University Hospital will continue as the principal teaching hospital of New Jersey Medical School (NJMS). Similarly, Robert Wood Johnson Medical School (RWJMS) will maintain its ties with Robert Wood Johnson University Hospital, subject to associated contractual agreements, and remain the principal teaching hospital of RWJMS.
We anticipate the integration will enhance our community impact in Newark and New Brunswick.
-
The physical locations of the medical schools will remain the same with two, comparable campuses in Newark and New Brunswick. No one campus will be subordinate to the other.
-
The integration will continue with the same day-to-day commitment to research, patient care, leadership in education, and community service on both future Rutgers School of Medicine campuses.
NJMS is not moving to New Brunswick or vice versa, nor are we allocating resources from either medical school inequitably.
The integration aims to retain and integrate both institutions’ talented faculty and staff. The combined expertise will foster collaboration and create a more dynamic and supportive academic environment.
Considerations for Prospective Students
Accordion Content
-
An integrated model of medical education will position the future Rutgers School of Medicine as one of the leading public medical schools in the country and create an unparalleled hub of biomedical and health sciences education, research, and clinical care. When complete, the integration envisions a medical school with a national reputation greater than the sum of its parts, amplifying Rutgers’ role as a leader in 21st-century medical education.
Closer collaboration on the educational mission will offer a broader scope and scale of teaching talent, learning content, and clinical experiences that benefit educators and learners. A unified medical school within Rutgers provides the opportunity to think big, innovate, enhance education, and attract more outstanding applicants from New Jersey and across the United States. For incoming students, benefits will include more research opportunities, more ways to collaborate, and more educational innovation.
-
An integrated medical school strongly identified with Rutgers University has the potential to broaden the national recognition of the excellent medical education programs and growing the research portfolios of each school. In addition, a combined medical school will rise in rankings and be more closely comparable to larger medical schools nationally.
-
In this cycle (i.e., applicants are applying to start medical school in July/August 2026), applicants should apply to both schools separately, as there are two admissions committees and both are accepting American Medical College Application Service (AMCAS) applications.
-
In the future, Rutgers School of Medicine will have one admissions committee and one interview process with an indicator of campus preference. Representatives from both campuses will interview and report to the Admissions Committee, which will report to the Executive Admissions Committee, which will make final decisions.
-
The future Rutgers School of Medicine curriculum is being developed. View the future Rutgers School of Medicine competencies. Many integrated experiences will launch even before accreditation, such as most of the core clerkships. The new Patient-Centered Medicine and Health Equity will launch in July 2025. Faculty have been highly engaged and thoughtful in this process.
-
To every extent possible, accepted applicants will be given the choice as to which campus they will join. The first offers of admissions will go out from the school and ask applicants to respond with the campus they will be joining. As the campuses fill, applicants will be offered a spot to a single campus with the offer being based on the applicant's stated preference and/or space.
-
No. The schools will join and keep the respective campus sizes the same.
-
If there were to be a delay in accreditation of the merged school, students would graduate from the medical school to which they were admitted. They would graduate from an LCME-accredited school.
Single Accreditation
To create a stronger medical education program that is well-equipped to meet the challenges of the future, the Rutgers University Board of Governors voted on July 10, 2023, to pursue a single medical school accreditation between New Jersey Medical School (NJMS) and Robert Wood Johnson Medical School (RWJMS). The integration of the medical schools will create two, comparable campuses under a single accreditation to be known as Rutgers School of Medicine.
The decision to integrate the medical schools was not made lightly, and it entailed a period of thorough evaluation, thoughtful consideration, and collaboration with our internal and external communities.
The primary objective of single medical school accreditation is to create a stronger, more innovative institution with enhanced educational opportunities, expanded research endeavors, and improved patient care. Simultaneously, this endeavor aims to elevate the reputation of the school.
The integration presents opportunities for growth, efficiency, and improved collaboration—and, most importantly, it will significantly enhance medical education for students. Integration will also improve and expand clinical care for our communities. The future Rutgers School of Medicine will continue to have a strong commitment to University Hospital in Newark and Robert Wood Johnson University Hospital in New Brunswick, with the relationship remaining unchanged.
Background
The delivery of health care continues to change and become more complex, and institutions that train the next generation of health care workers must not only be attuned to these changes, but be nimble enough to adapt to changes yet to come and ensure its students are positioned to meet the demands in this decade and beyond.
These dynamics, coupled with an ever-increasing health care worker shortage, represent the foremost reason why Rutgers Biomedical and Health Sciences (RBHS), now known as Rutgers Health, began to evaluate the educational structure of its medical schools.
In 2019, a 12-member Future of Academic Medicine Committee with equal representation from NJMS and RWJMS was formed to assess options and recommend ways in which further integration might benefit the medical schools and their students, and what the optimal structure might be.
After a year of deliberations, a thorough report on the future of academic medicine at Rutgers University was completed and presented to the Rutgers University Senate Executive Committee. Thereafter, the University Senate forwarded an extensive series of questions to prompt further deliberation and analysis.
In early 2022, following a postponement due to the COVID-19 pandemic, RBHS formally adopted a new strategic plan — “One RBHS: The Way Forward” — to guide the next five years. The plan’s Unifying Theme Goal 4: Enabling Systems and Structures focuses on assessing the effectiveness of our enabling systems, structures, and processes, with a specific call to “Evaluate options for further collaboration and potential consolidation of medical schools to synergize efforts and maximize outputs.”
With this prompt, along with the University Senate’s questions and a request from university senior leadership and governance bodies to reach some resolution, a logical starting point was established to revive the inquiry into the optimal structure for Rutgers’ medical schools.
University Senate Questions
-
- How would an integrated medical school handle student applications, admissions, tuition, and fees?
- Will student enrollment increase?
- What are the metrics for success in a proposed integration?
-
- What is the vision for a transformational undergraduate medical education curriculum/program?
- How would integration of the two medical schools align, reconcile, or reimagine the curriculum?
- How will an integrated medical school address clinical placements, pre-clerkship rotations, and clerkships?
- Will students be able to enroll in core classes and/or electives across campuses?
- Will there be a greater emphasis on distance/remote learning?
- Will students be expected to travel between campuses?
- How would an integrated medical school impact the current MD/PhD program?
- What are the metrics for success in a proposed integration?
-
- How will the integration of the medical schools ensure the campuses are co-equal?
- What will the impact of an integrated medical school be on our relationships with our primary hospital affiliates, namely University Hospital and the RWJBarnabas Health system?
- How will each campus retain its unique identity and strengths?
- How will faculty governance be implemented?
- What are the metrics for success in a proposed integration?
-
- How will an integrated medical school impact faculty recruitment?
- Nomenclature: What will be the name of the new school? The individual campuses?
- What will diplomas say?
- Will school departments be integrated under single chairs or will each campus retain a local chair?
- Will the integration result in higher medical school rankings?
- What is the anticipated cost of integrating the medical schools?
- What is the process to review and approve an integration of the medical schools?
- Who will be consulted: Students? Faculty? Alumni? Government officials? Senate? Boards? The Liaison Committee on Medical Education? Local communities? Hospital affiliates? Donors?
- Will each school/campus budget be held harmless and receive comparable funding once integrated, as in prior years?
- What are the budget, revenue, revenue cycle, and funds flow models for an integrated medical school?
- How will administrative systems such as information technology and grants management be integrated?
- What is the proposed administrative structure of an integrated medical school?
- What is the appropriate role and reporting relationship between medical school departments and RBHS research-based institutes vis-à-vis the integrated medical school?
- Will there be more or less faculty and staff in an integrated medical school?
- How will the integration improve administrative infrastructure on the two campuses?
- How will the clinical practices be organized in an integrated medical school?
- Will clinical services be provided locally, regionally, or both?
- What is the role of the dean?
- What is a proposed timeline to accomplish a medical school integration?
- How will parking and transportation between the two campuses be addressed?
- Will faculty be expected to travel between campuses?
- How will faculty promotions and tenure decisions be implemented?
-
- How will the integration improve research infrastructure on the two campuses?
- What is the appropriate role and reporting relationship between medical school departments and RBHS research-based institutes vis-à-vis the integrated medical school?
- How will access to research cores be addressed?
- Will integration enhance faculty competition for research funding or inhibit it as limited submission National Institutes of Health grant applications will only be one school applying versus two?
- What will be the impacts on federal grants and any limitations on aid for a larger school?
Evaluation Process
In September 2022, an announcement was made regarding the revival of an inquiry started in 2019 to determine the optimal level of integration between NJMS and RWJMS.
Committees of faculty, students, and staff from both schools were assembled to address key questions posed by the University Senate related to admissions, curriculum, and maintaining campus identity and culture. The current set of questions was derived from the original 350 University Senate questions presented in March 2020. Some of the original questions were duplicates, overlapped with other questions, and in some cases were related to topics timely only for 2020. The questions were consolidated, refined, and categorized in collaboration with the leadership of the University Senate during the summer of 2022.
The committees received RBHS Chancellor Brian Strom’s charge in October 2022 and began their work assessing ways in which enhanced cooperation and coordination might be advantageous for the medical schools, students, patients, and host communities.
NJMS Dean Robert L. Johnson, RWJMS Dean Amy Murtha, and Chancellor Strom were tasked with developing responses to those questions that are administrative in nature, and worked with the RBHS Office of Research to answer those questions particular to research.
ECG Management Consultants, a national consulting firm with expertise in academic health centers, was retained to facilitate the committees’ work. Janis Orlowksi, an expert on medical school administration who until recently was the chief medical officer at the Association of American Medical Colleges, also consulted on the project.
The committees completed their work and on January 31, 2023, Chancellor Strom presented the University Senate with the report that further develops a vision for the future of academic medicine at Rutgers University. This report represents the collective work product of numerous faculty, staff, students, community members, and administrators of NJMS, RWJMS, and RBHS and provides responses to the questions posed by the University Senate.
Evaluation Committees
Committees of faculty, students, and staff from both schools were assembled to answer key questions posed by the University Senate related to admissions, curriculum, and maintaining campus identity and culture.
-
Members
- Co-Chair: H. Liesel Copeland – Assistant Dean for Admissions, RWJMS
- Co-Chair: George F. Heinrich – Associate Dean, Admissions, NJMS
- Gloria A. Bachmann – Associate Dean, Women’s Health, RWJMS
- Joshua M. Kaplan – Associate Professor, Medicine, NJMS
- Natalia L. Kellam – Student, RWJMS
- Sonia C. Laumbach – Assistant Dean, Student Affairs, RWJMS
- Payal V. Shah – Student, NJMS
- Maria Soto-Greene – Executive Vice Dean, NJMS
- Carol A. Terregino – Senior Associate Dean, Education and Academic Affairs, RWJMS
- Danitza M. Velazquez – Assistant Professor, Pediatrics, NJMS
-
Members
- Co-Chair: Maria Soto-Greene – Executive Vice Dean, NJMS
- Co-Chair: Carol A. Terregino – Senior Associate Dean, Education and Academic Affairs, RWJMS
- Rashi Aggarwal – Vice Chair Residency Training Director and Professor, Psychiatry, NJMS
- Alla Fayngersh – Assistant Professor, Medicine, NJMS
- Meigra (Maggie) Myers Chin – Associate Professor, Emergency Medicine, RWJMS
- Amir George – Student, NJMS
- Brooke K. Phillips – Student, RWJMS
- Archana Pradhan – Associate Dean for Clinical Education, RWJMS
- Monica Roth – Professor, Pharmacology, RWJMS
- Michael E. Shapiro – Professor, Surgery, NJMS
- Ranita Sharma – Executive Vice Chair and Associate Professor, Medicine, and Residency Program Director, RWJMS
- Christin Traba – Associate Dean for Education, NJMS
-
Members
- Co-Chair: Charletta A. Ayers – Associate Professor, RWJMS
- Co-Chair: Melissa B. Rogers – Associate Professor, NJMS
- Shareif Abdelwahab – Student, RWJMS
- Bill Arnold – President and Chief Executive Officer, RWJMS
- Detlev Boison – Professor, Neurosurgery, RWJMS
- Alison L. Clarke – Program Coordinator, RWJMS
- C. Roy Epps – President/Chief Executive Officer, Civic League of Greater New Brunswick
- Carmen L. Guzman-McLaughlin – Senior Director, Administration, NJMS
- George Hampton – Retired Vice President, University of Medicine and Dentistry of New Jersey
- Michael Kelly – Associate Dean, Graduate Education, RWJMS
- Neil Kothari – Associate Dean, Graduate Medical Education, NJMS
- M. Chiara Manzini – Associate Professor, Child Health Institute of New Jersey, Neuroscience and Cell Biology, RWJMS
- Mary Maples – Interim President and Chief Executive Officer, University Hospital
- Ana M. Natale Pereira – Associate Professor, Medicine, NJMS
- J. Patrick O’Connor – Associate Professor, Orthopedics, NJMS
- Jon L. Oliver – Assistant Dean, Information Technology, School of Communication and Information
- Timothy Pistell – Student, NJMS
- Nikolaos Pyrsopoulos – Professor and Chief, Gastroenterology and Hepatology, NJMS
- Arnold Rabson – Director, Child Health Institute of New Jersey, RWJMS
- Frank Sonnenberg – Chief Informatics Officer, RWJMS
- Ian Whitehead – Professor of Microbiology, Biochemistry, and Molecular Genetics, NJMS
Evaluation Process Timeline
-
- January 2020: Future of Academic Medicine report explores the integration of NJMS and RWJMS
- Spring 2020: University Senate responds to the report with questions about integration. COVID-19 pandemic pauses the discussion
- January 2022: ONE RBHS 2022–2027 Strategic Plan calls for further evaluation
- October 2022: RBHS assembles three committees to address key University Senate questions
- November/December 2022: Committees develop related responses and recommendations for assigned questions with input from medical school communities
-
- January 2023: RBHS leadership synthesizes committee outcomes and presents report to University Senate
- Spring 2023: University Senate reviews and responds to report
- July 2023: University Board of Governors votes to pursue single accreditation
Documents and Reports
Chancellor's Letter to the Rutgers University Senate
July 7, 2023
Chancellor Strom addresses questions from the University Senate regarding the integration of Rutgers' two medical schools.
Attachments:
- Draft Proposed Resolution Establishing the future Rutgers School of Medicine
- Report to Rutgers University Board of Governors on the Development of Integrated Medical School Model
- Examination of Potential Residency Placement Concerns Due to Integrated Medical School
Report to the Rutgers University Senate: Envisioning the Future of Academic Medicine
January 31, 2023
Read the report presented to the University Senate on the future of academic medicine at Rutgers University.
Report to the RBHS Chancellor: The Future of Academic Medicine at Rutgers
January 10, 2020
Read the report to RBHS Chancellor Brian Strom from the Future of Academic Medicine Committee.
Follow Us
New Jersey Medical School and Robert Wood Johnson Medical School are in the process of preparing for full Liaison Committee on Medical Education (LCME) accreditation to create the future Rutgers School of Medicine.
Timeline- On-site survey visit: January 11–13, 2027
- Earliest date for possible accreditation: June 2027